Abstract
Background: Acute Myeloid Leukemia (AML) outcomes are dependent on leukemia-specific factors, such as cytogenetics and patient-specific factors, such as age and performance status. Racial and socioeconomic disparities have become apparent with self-reported African American race associated with poor survival in AML pts < 60 years (y) of age. We analyzed in-hospital death among AML-related hospitalizations and evaluated differences in sociodemographic characteristics, focusing on the effect of age and race.
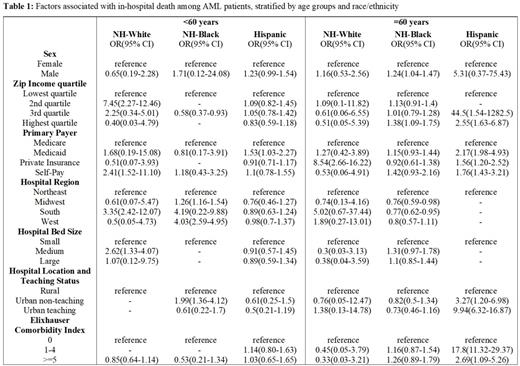
Methods: We conducted a retrospective cohort study using the Nationwide Inpatient Sample (HCUP-NIS), the largest all‐payer database of hospital admissions in the United States, from January 1 st, 2009 through December 31 st, 2018. The study sample consisted of AML-associated hospitalizations of patients aged 18 years of age and older, identified on the basis of the presence of any ICD-9 and 10 codes indicative of AML We categorized patients' ages in groups of <60 y and ≥ 60 y. Ethnicity was initially stratified by reported ethnicity (Hispanic, Non‐Hispanic), and the Non‐Hispanic group was subdivided into White, Black, or other. The primary payer for the hospitalization was classified. As a proxy for socioeconomic status, the HCUP-NIS provides zip‐code‐level estimates of median household income, grouped into quartiles based on the patient's residence. Hospital factors included census region, bed size, and hospital type. Patients' comorbidity status was captured using Elixhauser Comorbidity Index (0, 1-4, 5+). Outcome of interest was in-hospital death. Among different age groups and ethnic groups of patients with AML, we used survey logistic regression to generate adjusted odds ratios (aORs) and 95% confidence intervals (CIs) that measured the independent associations between various patient hospitalization characteristics and inpatient death. We adopted a 5% type I error rate for the calculation of CIs, and used appropriate survey weighting to generate national prevalence estimates considering the complex sampling design of the NIS. Statistical analyses were performed using R (version 3∙6∙1) and RStudio (Version 1∙2∙5001).
Results: Of 662,417 AML-related hospitalizations, 57.6% were in patients ≥60 y. Of AML-related hospitalizations in patients <60 y, 61.6% were in NH-White patients, 11.2% were in NH Blacks, and 11.7% were in Hispanics. Of AML-related hospitalizations in patients ≥60 y, 74.6% were in NH-Whites, 7.3% in NH-Blacks and 5.4% in Hispanics. Analysis of in-hospital death among AML-related hospitalizations, stratified by race/ethnicity revealed increased in-hospital death among male NH-Black AML patients ≥ 60 y as compared to NH-Black females in the same age group (OR 1.24; CI 1.04-1.47) and an increased in-hospital death among Hispanic patients ≥ 60 years with comorbidities relative to their counterparts in the same age group without comorbidities (OR 17.8; CI 11.32-29.37 for Elixhauser Comorbidity Index 1-4 and OR 2.69; CI 1.09-5.26 for Elixhauser Comorbidity Index ≥5). Differences in income, primary payer, hospital region, size, location or teaching status were not associated with in-hospital death among AML patients stratified by race/ethnicity. See Table 1.
Conclusions: We found a significant increase in in-hospital death among Hispanic patients ≥ 60 y with comorbidities relative to their counterparts in the same age group without comorbidities. Yet, comorbidities did not appear to have a statistically significant impact in mortality for patients of other race/ethnicity or those <60 y. It is plausible that the relationship between comorbidities and re-hospitalizations might be impacting our data. Previous work not specific to acute myeloid leukemia has shown that higher comorbidity is associated with an increased risk of readmission. Since our data was based on AML-related hospitalizations rather than patients with AML, it is possible that we are dealing with a false negative error because of patients with comorbidities being readmitted more. The lack of cytogenetic data in NIS is another notable limitation to our work. Nonetheless, we have found striking differences in the outcomes of elderly Hispanic comorbid patients and further evaluations are needed for correlation and to identify areas of optimization in their care.
Mims: Incyte: Research Funding; AVEO: Research Funding; Pfizer: Research Funding; IDEC: Current holder of individual stocks in a privately-held company; Celgene: Research Funding; Biogen: Current holder of individual stocks in a privately-held company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal